Coronavirus and behaviour
In this post I want to roughly synthesise what I think I know about the UK government’s response to the coronavirus outbreak, the public reasoning behind it, and whether I think it will work. I am attempting to be as clear as I can about my assumptions so that people can spot my mistakes, or at least understand my reasoning.
(1) The virus itself.
(a) Without changing behaviour, we will see significant total caseloads
Coronavirus appears to be transmissible via direct contact and airborne spread, as well as from contact with unclean surfaces. People may be mildly contagious when they are asymptomatic. The disease is spreading “easily and sustainably” in the USA, and has already done so in China and Italy. Each person with the disease can be expected to infect roughly 2.28 other people, although this figure is dependent on policy decisions.
The UK currently expects the virus to reach between 50% and 80% of the population. Germany provides a similar upper-end estimate of 70%.
(b) Mortality will be low overall, but higher in sub-groups
The total case-fatality rate in China appears to be around 2.3%, but varies significantly with age. Those aged 70-79 face a case mortality rate of 8%, and those aged 80+ one of 14.8%. Those with pre-existing medical conditions are also at risk.
(c) Approximately 10% of cases will require hospital treatment.
The CDC suggests that 80% of infections are mild or asymptomatic — a category which still allows for “mild pneumonia” — 15% are ‘severe infections requiring oxygen’, and 5% are ‘critical infections requiring ventilation’. Italian doctors have stated approximately 10% of cases are admitted to intensive care.
(d) The pattern of infections rises to a peak then drops. Under business as usual, the peak of infections is 10 to 14 weeks away.
This has been publicly stated by the UK chief medical officer. We can expect to see 50% of all cases in a three week period, and 90% over a longer nine week window.
(e) Patients can take a period of ~3 weeks to recover.
Drawn from examples here and here. Patient groups may not be representative but a 2-3 week treatment period does not seem unreasonable.
Conclusions
i) Somewhere between 33 million and 53 million people will be infected in the UK
ii) Some 5 to 8 million could require hospitalisation assuming all severe infections are hospitalised.
iii) If we assume a less aggressive treatment regime targeting only the 5%, this leaves us with 1.66 to 2.65 million patients requiring hospital treatment.
iv) Implied peak load is then somewhere between 2.5 million and 4 million people requiring hospital treatment over a 3 week window, or 830,000-133,000 on the less aggressive assumption.
v) Given the duration of hospitalisation observed elsewhere, a substantial number of these cases will require simultaneous treatment.
(2) Health system capacity
(a) The NHS has approximately 140,000 hospital beds in England, 20,000 in Scotland, and 11,000 in Wales.
(b) There are around 3,700 critical care beds in England. For patients incapable of breathing even with mechanical assistance, 15 beds have provision for providing oxygen.
Assuming a similar proportion of around 3% of Scottish and Welsh beds allocated to critical care, let’s say a total in the region of 4,500.
(c) 80% of intensive care beds are occupied.
(d) People will continue to get sick or injured while the outbreak is ongoing
(e) Under a scenario where patient numbers continue to grow, we will likely be forced to triage patients.
Under normal circumstances we would expect significantly better outcomes for coronavirus than we are likely to experience. It seems plausible that a majority of the deaths we will see will follow because the virus has the capacity to collapse the health system.
Italy is already triaging patients, and the UK’s 2011 pandemic preparedness strategy suggested that in a high impact scenario of the sort we might expect to see that this would follow.
(f) An overloaded health system will increase the mortality rate associated with the virus
Patients who might otherwise have recovered will not do so.
Conclusions.
i) The most optimistic peak load assumptions require a multiple of the total beds available to the NHS.
ii) If every hospital bed were turned over to treating coronavirus patients, and another 100,000 conjured up from nowhere, we would still be well short of the required total.
iii) Without closing the gap between capacity and demand, patients who would otherwise live will die. We will see a death rate potentially on par with that seen in Italy.
(3) Closing the gap between capacity and infections
(a) Significantly adding to the total number of beds available is not a short-term project.
We will not be able to increase capacity to meet demand. We will have to lower demand to meet capacity.
(c) We don’t have the tools to accurately track the spread of the virus and we are under-counting existing cases.
We can infer this from two points. The first is that the UK can currently carry out around 1,500 tests per day. The NHS is working to increase capacity, but this is what we have to work with for now. The response to this was (initially at least) to limit testing to those who had returned from certain infected areas – but not all such locales – and the people who knew they had been in contacted with the sick.
Combine this restrictive regime with fact (1a) and you have a perfect scenario for community circulation; an infected person coughs in an underground carriage, spreading the disease to people who don’t know about their recent movements, and the virus is free to circulate untested. Given that some of these people will arrive in hospitals to be treated, we could expect to see the disease take hold among vulnerable people and their visitors.
The second observation is simply the suspiciously high number of celebrities testing positive. Individuals in this group are more able to afford scarce testing kits; NBA team the Utah Jazz, for instance, got hold of 58 testing kits to check its employees after a player fell ill. Those 58 tests represented almost 0.4% of all the tests conducted in the USA.
While high-net-worth individuals are more likely to travel or engage with large numbers of people — raising their risk of exposure — it’s unlikely that this would sufficiently explain the high numbers testing positive. It is also unlikely that the rate of the illness is massively higher in this group than in the general population; we are missing cases.
The government agrees; the official estimate is that there are somewhere between 5,000 and 10,000 people infected. As we can’t keep up with demand for tests, only those with serious symptoms will be tested.
The likely mechanism for tracking total infections will be back-engineering estimates from positive tests on hospitalised patients. Given the uncertainty over precisely how dangerous the disease is, the error margins on these figures could be quite substantial.
(c) Containment may no longer be possible.
This follows from the above. Given that the disease is in community circulation and our lack of testing ability, we will not be able to root it out.
With that said, containment does not appear to have been the plan in the first place. Going back to the 2011 strategy (here), the rough timeline of measures anticipated was to try and spot the arrival of the pandemic, then actively find and isolate cases. Once in the community, there’d be a slow ramping up of localised public health measures.
Attempting to prevent as many infectious arrivals as possible – as successfully achieved by Taiwan and Singapore – was not really considered. A 90% reduction in the passenger inflow would delay the peak of the disease by one to two weeks, and a 99.99% reduction by two months or so.
This, I must say, seems questionable in the light of the continued success of countries with high flows from China in reducing exposure to the disease. Reducing the total number of sick arrivals, or effectively screening at airports, seems like a plausible mechanism for reducing the number of unknown cases in the community.
(d) Reducing the total number of cases was highly desirable, but spreading the load of cases is an important secondary priority.
If you can’t prevent people catching coronavirus, you can at least try to make sure they don’t all catch it at the same time. We have moved too slowly to effectively contained the disease, but that does not mean movement now is worthless.
(e) Lowering patient numbers could be achieved through social distancing as well as through stricter lockdowns.
The Chinese government lockdown has successfully arrested the rate of increase in coronavirus cases. Singapore, Taiwan, and Hong Kong have managed to avoid these measures by acting rapidly to reduce the inflow of cases through travel restrictions, quarantining existing cases, and encouraging reduced contact.
These measures have involved — deep breath — mandatory and enforced quarantine or isolation for returning travellers, screening at all points of entry, banning flights from heavily affected regions or from any but essential areas, tracking the movements of infected people through financial data and other records, suspending large gatherings, encouraging working from home, conducting daily temperature screenings in workplaces, public education on hygiene, encouraging organizers to defer or cancel events, distributing surgical masks to reduce the airborne spread of the virus, conducting temperature screenings at points of entry, closing schools, and so on.
Each country has taken a different combination of measures, but the total effect in each has been similar.
(f) Reducing the rate of infection is more valuable when done early.
This observation follows from thinking through the nature of any time-varying Markov process. What we are concerned about is the is the rate of healthy people falling sick in a period, the number requiring hospital care simultaneously, and the number who will die. These are not independent; the more people who fall ill, the higher the peak load. The higher the peak load, the higher mortality.
Given the nature of exponential growth, it’s better to implement measures to reduce the first variable early than it is to do so late.
Conclusions
i) We need to close the gap between capacity and peak demand; as we can’t raise the first significantly, we need to lower the second.
ii) We can’t contain the virus as we don’t have sufficient testing capacity, and it is already too widely spread in the community.
iii) Measures to lower the total spread are still available, as are those to increase the temporal dispersion of the caseload.
iv) These measures have a correspondingly larger effect when implemented early.
(4) What the UK is doing
(a) For now, almost nothing.
The current government tactic has been termed the ‘delay’ phase. This effectively consists of asking people politely to wash their hands properly, and to self-isolate for seven days if they show symptoms.
(b) Some light social distancing will be introduced in the next two weeks.
The government also intends to ask the elderly and otherwise vulnerable to consider self-isolation for their own good.
(c) The government’s strategy appears to be based on an assumption generated by a tenuous application of behavioural science.
The logic behind delaying more effective social distancing is that there is a risk of people suffering from “self-isolation fatigue“, leaving their containment at the height of the disease period with the result that it spreads more rapidly.
This has been described as the result of epidemiological modelling, but I think this is probably incorrect; this decision is the output of a model which took in as an input the idea that people would breach isolation after a certain point.
(d) It is not immediately apparent that this assumption is true.
Singapore, Taiwan, and Hong Kong are our test-cases for the extended application of social distancing. So far things appear to be working rather well.
The assumption behind the government model is that you can’t maintain this forever, so it’s best to try and introduce it for (say) four to six weeks when you think you can have the largest impact on the peak of the virus.
It is not immediately apparent that an extended regime of social distancing over a period of months would prove unsustainable. We know that the effect of social nudges can decay over time (example), and that people can tune out messages they’ve heard before.
But all of this is incredibly dependent on context; a new letterhead on a tax letter may be rather less effective than the image of a tumour on a packet of cigarettes. In this case, we are seeing a large change in the incentives to change behaviour (“don’t kill granny”) and a practically unique context. Relying on international evidence from previous outbreaks (such as the swine flu pandemic) displaying effect attenuation, for instance, does not quite account for the comparative predicted severity of current circumstances – and indeed that research also shows that reductions in transmission were achieved, as does research on purely behavioural responses from 1918.
Perhaps more importantly, the idea that interventions are once-and-done is deeply curious. If we were to intervene now, see a rise in cases as fatigue set in, and then repeat the intervention as death tolls begin to rise, it is plausible that there would be a degree of ‘resetting’.
(d) It is not apparent that we will be able to time measures effectively
This is an interesting strategy given that we will be restricting testing to hospital cases, and that demand for tests may well outstrip our capacity to administer them. The idea is that there is an optimal time period where action will have the greatest effect on demand. Act before, and the effect will be lower. Act after, and it will be too late.
But timing for that window is incredibly dangerous strategy when you can’t monitor the spread. The whole thing is very reminiscent of the ‘catching a falling knife’ analogy to timing buys in falling stock markets; if you can pull it off then you will profit substantially, but you risk some truly catastrophic losses.
(e) Measures which do not ‘flatten the peak’ but merely delay it are still incredibly valuable.
It is likely that we are still some way off a functioning vaccine, manufactured and administered at scale. But with each week that goes by we are gathering data on the best approach to treating the virus, as well as improving the odds that a breakthrough will occur in the interim. Measures which delay the viral peak one to two months should be welcomed, not ignored.
Update 14/03/2020: Fixed language from ‘move viral peak forwards’ to ‘delay’.
(f) The government is not thinking at the margin
Both the 2011 pandemic response plan and the government’s current rhetoric is marked by a dismissive attitude towards measures which would ‘only’ reduce or delay the peak by a small period.
The government believes that encouraging people to wash their hands and self-isolate if symptomatic could cut the peak case-load by 20%.
Restricting mass gatherings, on the other hand, is not worthwhile, as it would only cut peak case-load by 5%. And of course people would socialise in smaller groups, swapping football grounds for pubs. Besides, as the 2011 plan sets out, these are a “useful indicator of normality”. Right. Here’s the thing; this isn’t normal, and with hospitals vastly over capacity cutting the case load by 5% could make a big difference to a lot of people, and removing mass events limits the degree to which large and unexpected clusters of transmissions can occur, making tracking easier and the infection total lower.
School closures are not planned, again following the 2011 document (which suggested localised closures in earlier phases, dropped entirely once the pandemic took hold). The government has shown no interest as “children off school would end up socialising anyway or spending time with grandparents”. Quite why infecting 20-30 is preferable to infecting 4-5 is not immediately apparent, and what worries me about this is the binary thinking it implies: ‘if you infect one person, you may as well infect many’. Anything we can do to reduce transmissions at this point is valuable, and the government’s own evidence is that it would reduce the peak load by 10-15%. The idea that school closures would affect care and health workers is also a non-starter; there is always the option of keeping them open for related students only.
Broadly, this attitude is curious. Firstly, the combination of many small measures — particularly those where the government is in a position to effectively enforce changes in behaviour — can sum to a significant change in overall outcomes. Secondly, delaying the peak of the virus is in itself incredibly valuable.
(g) The rest of the world is entirely out of step.
As covered above, the rest of the world has adopted a very different approach to that taken by the UK. Either our researchers have identified a pattern which China, Singapore, South Korea, Italy, France, Australia, Iceland, and so on have failed to find or consider, or we are basing our policy on a degree of confidence in the available evidence on behaviour which is clearly not shared by the rest of the world.
France is closing all schools and universities, as is Ireland. Japan has closed its schools. Iceland and France have banned gatherings over 100 people, and Australia over 500. Italy has progressed from a national quarantine to something akin to a total lockdown of activity, banning public gatherings, preventing non-urgent travel, limiting opening hours, and encouraging citizens to limit social contact.
And the UK is waiting to see what happens.
If you turn up in an empty lecture theatre at 9am, it’s entirely possible the professor and the rest of your classmates have mistakenly headed to the wrong room. It’s just rather more likely that you’re wrong. Other countries have perfectly competent scientists and policy makers. In many cases I suspect theirs may be rather better. Precisely how confident are we in Public Health England?
(h) The long term nature of the plan is also dubious.
The government’s concern is that when you end social distancing — assuming it would end prior to the production of a viable vaccine — you then experience an increase in cases once more. By having people infected over a short (but not too short) window, you may be able to acquire a degree of herd immunity, whereby enough of the population are resilient to the disease that it will not recur.
We can probably assume that under the government’s plan enough people will be sick for this to work in theory — 60% of the population, for the record — but it is not immediately clear that long term immunity can actually be acquired. There are also early suggestions that the disease can cause long term damage to lung function, the central nervous system, and other systems of the body.
Conclusions
i) The government’s strategy is based on an at-best-dubious application of behavioural science not borne out by observations elsewhere.
ii) The idea that interventions can be timed precisely enough to maximise impact is at odds with our lack of capacity for accurately tracking spread.
iii) There appear to be options open which would substantially reduce the peak caseload if taken in combination, and potentially the total number of infections.
iii) The plan to acquire herd immunity risks long-term health consequences and is not guaranteed to actually work.
iv) Other countries with access to expertise have adopted a very different approach.
Summary
We’re embarking on a novel experiment in the response to pandemic diseases based on unclear behavioural assumptions, an evidence base cobbled together from context-dependent results likely drawn from very different circumstances, and without an understanding of the long-term effects of the disease in play.
While total containment might not be possible it is not clear that the total number of infected could not be dramatically reduced by following a different strategy. Options taken to delay the peak for as long as possible would also be valuable, as we could gather information on viable treatments.
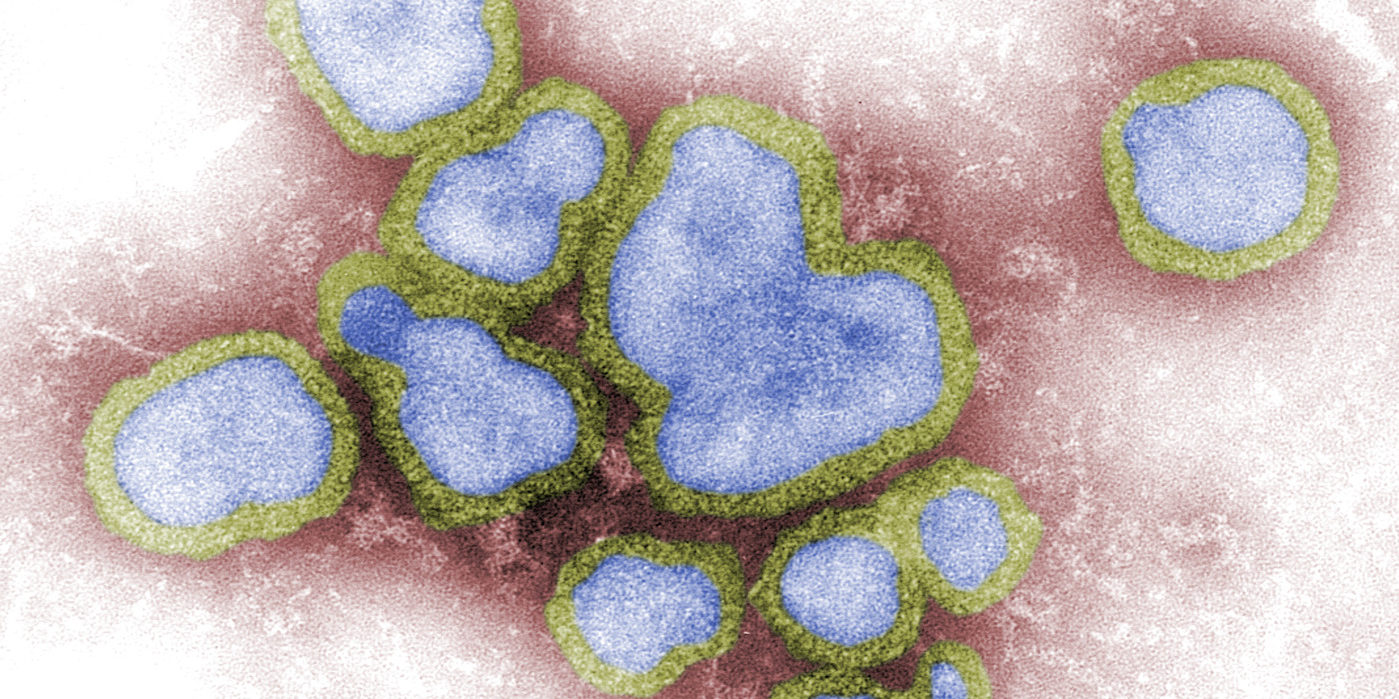
Header image courtesy of Sanofi Pasteur on Flickr, taken by CDC/ F. A. Murphy, used under a creative commons license.